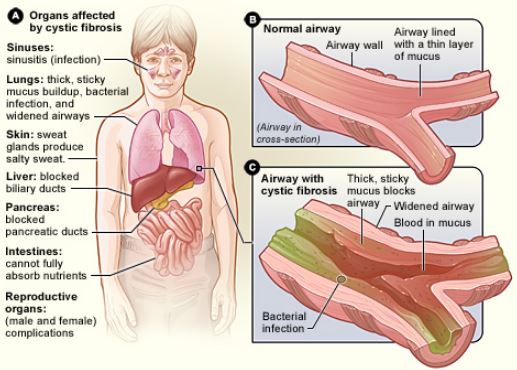
Cystic Fibrosis (CF) is a complex genetic disorder that predominantly impacts the respiratory and digestive systems, leading to thickened mucus secretions and a range of associated health challenges. For those diagnosed with CF, understanding the intricacies of the condition is paramount. While CF presents a myriad of challenges, it’s not insurmountable.  With the right knowledge, tools, and practices, individuals can effectively manage their symptoms, reduce complications, and enhance their quality of life. This guide aims to be a beacon, shedding light on the multifaceted aspects of CF management. From the nuances of airway clearance techniques to the importance of mental well-being and the intricacies of nutritional needs, we’ll provide a holistic overview, offering actionable insights and guidance for those navigating the daily challenges of life with CF. Here’s a comprehensive list of things that a person with CF should know to maintain their health:
With the right knowledge, tools, and practices, individuals can effectively manage their symptoms, reduce complications, and enhance their quality of life. This guide aims to be a beacon, shedding light on the multifaceted aspects of CF management. From the nuances of airway clearance techniques to the importance of mental well-being and the intricacies of nutritional needs, we’ll provide a holistic overview, offering actionable insights and guidance for those navigating the daily challenges of life with CF. Here’s a comprehensive list of things that a person with CF should know to maintain their health:
1. Regular Medical Check-ups:
For individuals with CF, consistent medical supervision is paramount to monitor disease progression, adjust treatments, and ensure optimal health. Here’s a detailed breakdown:
-
Pulmonologist Visits:
- Frequency: Most CF patients see their pulmonologist every 1-3 months. The frequency can vary based on the individual’s health status.
- Purpose: To assess lung function, listen to the lungs, and adjust treatments as necessary.
-
Lung Function Tests:
- Spirometry: Measures the amount and speed of air a person can inhale and exhale. It’s a primary tool to assess how well the lungs are working.
- Lung Volume Tests: Measure the total volume of air the lungs can hold, helping to identify any restrictions.
- Gas Diffusion Tests: Assess how well oxygen passes from the lungs into the bloodstream.
-
Imaging Studies:
- Chest X-rays: Provide images of the lungs and can detect complications like lung infections or structural abnormalities.
- CT Scans: Offer more detailed images and can identify issues like bronchiectasis or mucus blockages.
-
Blood Tests:
- Complete Blood Count (CBC): Monitors overall health and detects disorders like anemia or infection.
- Liver Function Tests: Ensure the liver is working correctly, as CF can sometimes affect liver health.
- Vitamin Levels: Especially important for fat-soluble vitamins (A, D, E, K) as CF can affect their absorption.
-
Sputum Cultures:
- Purpose: Identify which bacteria or fungi are present in the mucus. This helps in tailoring antibiotic treatments.
- Frequency: Regularly done, especially if there’s a change in symptoms or during routine check-ups.
-
Bone Density Scans:
- Purpose: CF can affect bone health, making individuals more prone to osteoporosis or fractures. These scans assess bone strength.
- Frequency: Typically done annually or biannually, especially in adults with CF.
-
Nutritional Assessment:
- Dietitian Visits: Regular consultations ensure that individuals with CF are getting the nutrients they need, as the condition can affect digestion and absorption.
- Growth and Weight Monitoring: Especially crucial for children and adolescents to ensure proper growth and development.
-
Endocrinologist Visits:
- Purpose: CF-related diabetes is the most common comorbidity in adults with CF. Regular monitoring of blood sugar levels and endocrine health is essential.
-
Annual Flu Shots and Vaccinations:
- Staying up-to-date with vaccinations is vital to prevent respiratory infections that can exacerbate CF symptoms.
2. Airway Clearance Techniques (ACTs):
Airway clearance is a cornerstone of CF management, aimed at removing the thick mucus from the lungs. Here are the various ACTs in detail:
-
Chest Physiotherapy (CPT):
- Manual CPT: Involves another person clapping on the patient’s chest and back using cupped hands. The patient is positioned in ways that use gravity to help drain the mucus.
- Mechanical CPT: Devices like the ThAIRapy Vest produce high-frequency vibrations to the chest, shaking the mucus loose.
-
Positive Expiratory Pressure (PEP) Devices:
- Devices like the Flutter or the Acapella combine vibration with positive expiratory pressure. When exhaled into, they create vibrations and back pressure, aiding mucus dislodgment.
- Typically repeated in cycles, interspersed with periods of normal breathing.
-
High-Frequency Chest Wall Oscillation (HFCWO):
- An inflatable vest connected to a machine is worn. The machine vibrates the vest at high frequencies, shaking the chest wall to dislodge mucus.
- Sessions typically last 20-30 minutes.
-
Autogenic Drainage (AD):
- A self-administered technique where breathing is controlled to move mucus from smaller to larger airways. It involves three phases: deep inhalation, breath-holding, and slow, complete exhalation.
-
Active Cycle of Breathing Technique (ACBT):
- Combines deep breathing, huffing, and coughing. Deep breathing gets behind the mucus, huffing moves it closer to the mouth, and coughing expels it.
- This cycle is repeated until the airways feel clear.
-
Aerobic Exercise:
- Physical activities that increase heart rate can also assist in mucus clearance due to increased airflow during exercise. This natural method complements other ACTs.
3. Medications for Cystic Fibrosis:
-
Mucolytics:
- Dornase alfa (Pulmozyme): A recombinant DNA enzyme that breaks down the DNA in mucus, making it less thick and sticky. It’s inhaled once or twice daily using a nebulizer.
- Hypertonic saline: A saline solution that helps draw water into the airways, making the mucus thinner and easier to cough up. It’s typically nebulized and inhaled.
-
Bronchodilators:
- Albuterol, Levalbuterol: These are short-acting bronchodilators that relax the muscles around the airways, allowing them to open up. They are often used before other inhaled treatments to enhance their effectiveness.
- Salmeterol, Formoterol: Long-acting bronchodilators that provide extended relief, usually up to 12 hours.
-
Anti-Inflammatories:
- Ibuprofen: High doses of this over-the-counter NSAID can reduce lung inflammation in some CF patients. Dosage and frequency should be closely monitored due to potential side effects.
- Azithromycin: While primarily an antibiotic, it’s used in CF for its anti-inflammatory properties, especially in patients with chronic Pseudomonas aeruginosa infections.
-
Antibiotics:
- Tobramycin (TOBI, Bethkis): Inhaled antibiotic specifically for Pseudomonas aeruginosa infections.
- Aztreonam (Cayston): Another inhaled antibiotic targeting Pseudomonas.
- Ciprofloxacin and Levofloxacin: Oral or intravenous (IV) antibiotics that treat a variety of bacterial infections.
- Colistimethate (Colistin): Inhaled or IV antibiotic for multi-drug resistant bacteria.
-
Other Medications
- CFTR Modulators: These target the defective CFTR protein, addressing the root cause of CF.
- Ivacaftor (Kalydeco): Enhances the function of the CFTR protein at the cell surface.
- Lumacaftor/Ivacaftor (Orkambi): Lumacaftor helps move the CFTR protein to the cell surface, while Ivacaftor enhances its function.
- Elexacaftor/Tezacaftor/Ivacaftor (Trikafta): A combination therapy that has shown significant improvements in lung function for many with CF.
- Pancreatic Enzyme Replacement Therapy (PERT):
- Creon, Zenpep, Pancreaze, Pertzye: These are oral capsules containing digestive enzymes that help CF patients digest and absorb food. They are taken with every meal and snack.
- Vitamin Supplements: Due to malabsorption, CF patients often need additional vitamins, especially the fat-soluble ones (A, D, E, K).
4. Nutrition for Cystic Fibrosis:
Proper nutrition is essential for individuals with CF, as it supports growth, boosts the immune system, and helps the body fight infections. Due to the body’s malabsorption of nutrients, specific dietary adjustments are often required.
- Caloric Intake:
- Increased Needs: Many with CF require more calories than the average person due to increased energy expenditure and malabsorption.
- High-Fat Diet: A diet rich in healthy fats can help meet the increased caloric needs. This includes avocados, nuts, seeds, and fatty fish like salmon.
-
Pancreatic Enzyme Replacement Therapy (PERT):
- Digestive Aid: Most people with CF produce insufficient digestive enzymes. PERT involves taking enzyme capsules with meals and snacks to help break down and absorb food.
- Dosage: The amount and type of enzymes vary among individuals. It’s crucial to work with a dietitian to determine the right dosage.
-
Vitamins and Minerals:
- Fat-Soluble Vitamins: Due to fat malabsorption, there’s often a deficiency in vitamins A, D, E, and K. Supplements can help meet the required levels.
- Salt: People with CF lose more salt in their sweat. Including salty snacks or adding salt to meals can help compensate for this loss.
- Bone Health: Calcium and vitamin D supplements might be recommended to support bone health, as CF can increase the risk of osteoporosis.
-
Hydration:
- Staying hydrated helps thin the mucus, making it easier to clear from the lungs. Drinking plenty of water throughout the day is essential.
-
Dietary Fiber:
- A diet rich in fiber can help prevent constipation, a common issue in CF due to thickened digestive secretions. Foods like whole grains, fruits, and vegetables are good sources.
-
Specialized Nutrition Plans:
- Tube Feeding: Some individuals might require supplemental tube feeding to meet their nutritional needs, especially during illness or periods of decreased appetite.
- Diabetes Management: CF-related diabetes is a common complication. Managing blood sugar levels through diet becomes crucial, often requiring a balance of carbohydrates, proteins, and fats.
-
Gastrointestinal Issues:
- Gastroesophageal reflux disease (GERD) and other gastrointestinal issues are common in CF. Dietary modifications, such as smaller, frequent meals and avoiding spicy or acidic foods, can help manage symptoms.
-
Collaborative Care:
- Regular consultations with a registered dietitian specializing in CF can help tailor a nutrition plan, monitor growth and weight, and adjust dietary recommendations as needed.
5. Exercise for Cystic Fibrosis Patients:
Exercise plays a pivotal role in the management of CF. Not only does it help in improving lung function by clearing mucus, but it also enhances overall strength, stamina, and mental well-being.
Benefits of Exercise for CF Patients:
- Lung Function: Exercise increases ventilation and helps clear mucus from the airways, reducing the risk of infections.
- Bone Health: CF can lead to decreased bone density. Weight-bearing exercises can help improve bone strength.
- Muscle Mass: Maintaining muscle strength is crucial, especially since CF can lead to muscle wasting.
- Mental Health: Exercise releases endorphins, which can help combat depression and anxiety often associated with chronic illnesses.
- Improved Digestion: Physical activity can aid in digestion and reduce the risk of constipation.
Types of Exercises:
- Aerobic Exercises:
- Purpose: Enhance cardiovascular health, improve lung capacity, and aid in mucus clearance.
- Examples: Walking, jogging, cycling, swimming, and dancing.
- Tips: Start slow and gradually increase intensity. Ensure adequate hydration.
-
Strength Training:
- Purpose: Build muscle mass, improve bone density, and enhance overall strength.
- Examples: Weight lifting, resistance band exercises, and bodyweight exercises like push-ups and squats.
- Tips: It’s essential to maintain proper form to avoid injuries. Consider working with a physical therapist or trainer familiar with CF.
-
Flexibility and Stretching:
- Purpose: Enhance joint mobility, reduce muscle stiffness, and improve posture.
- Examples: Yoga, Pilates, and regular stretching routines.
- Tips: Focus on breathing during stretches. Incorporate dynamic stretches before workouts and static stretches post-workout.
-
Balance and Coordination:
- Purpose: Improve stability, reduce the risk of falls, and enhance functional movement.
- Examples: Tai Chi, balance ball exercises, and agility drills.
- Tips: Start with basic exercises and progress to more challenging ones as balance improves.
-
Breathing Exercises:
- Purpose: Strengthen respiratory muscles, improve lung function, and aid in mucus clearance.
- Examples: Diaphragmatic breathing, pursed-lip breathing, and the Buteyko method.
- Tips: These exercises can be incorporated into daily routines and can be especially beneficial during exacerbations.
Considerations for CF Patients:
- Hydration: Due to increased salt loss in sweat, it’s crucial to stay well-hydrated during and after exercise.
- Infection Prevention: If exercising in public spaces like gyms, be cautious about hygiene to avoid exposure to germs.
- Consultation: Always consult with a healthcare professional before starting a new exercise regimen. They can provide guidance tailored to individual health needs.
6. Avoid Infections:
-
Hand Hygiene:
- Washing: Use soap and water, scrubbing for at least 20 seconds, especially after coughing, sneezing, or touching potentially contaminated surfaces.
- Sanitizers: If soap and water aren’t available, use an alcohol-based hand sanitizer with at least 60% alcohol.
-
Environmental Precautions:
- Clean Living Spaces: Regularly disinfect surfaces, especially high-touch areas like doorknobs, light switches, and remote controls.
- Air Quality: Consider using air purifiers to reduce airborne pathogens. Ensure good ventilation in living spaces.
- Avoid Mold: Mold can exacerbate respiratory issues. Use dehumidifiers in damp areas and fix any water leaks promptly.
-
Personal Protective Equipment (PPE):
- Masks: Wear masks in crowded places or areas with a high risk of airborne pathogens.
- Gloves: Useful when cleaning or coming into contact with surfaces in public areas.
-
Vaccinations:
- Stay up-to-date with recommended vaccines, especially the flu shot and pneumococcal vaccines, to prevent respiratory infections.
- Discuss with your healthcare provider about any additional vaccines that might be beneficial.
-
Limit Exposure:
- Avoid Sick Contacts: Stay away from individuals who are ill, especially those with respiratory symptoms.
- Crowded Places: During flu season or outbreaks of respiratory illnesses, limit time in crowded areas.
-
Safe Food Practices:
- Cooking: Ensure foods are cooked to the recommended temperature to kill pathogens.
- Storage: Store perishable items in the refrigerator promptly. Be aware of expiration dates.
- Raw Foods: Wash fruits and vegetables thoroughly. Be cautious with raw or undercooked seafood and meats.
-
Water Safety:
- Drinking Water: Ensure your drinking water source is clean. Consider using water filters if unsure about water quality.
- Avoid Stagnant Water: Stagnant water can harbor harmful bacteria. Avoid activities in stagnant ponds or lakes.
-
Regular Health Monitoring:
- Symptom Tracking: Be vigilant about any new or worsening symptoms and seek medical advice promptly.
- Regular Check-ups: Even if feeling well, regular visits to the healthcare provider can help in early detection and management of potential infections.
-
Medication Adherence:
- If prescribed antibiotics or other medications to prevent or treat infections, take them as directed and complete the full course.
7. Stay Away from Smoke and Pollutants:
For individuals with CF, the respiratory system is already compromised, making it even more crucial to avoid any additional irritants that can exacerbate symptoms or lead to further complications. Here’s a detailed breakdown:
-
Tobacco Smoke:
- Firsthand Smoke: If you have CF, it’s imperative never to smoke. Smoking can severely worsen lung function and accelerate lung damage.
- Secondhand Smoke: Exposure to others’ smoke can be just as harmful. Ensure that your living environment is smoke-free. Politely ask friends and family not to smoke around you or in your home.
-
Air Pollution:
- Outdoor Pollutants: Urban areas can have high levels of pollutants. On days when air quality is poor, it’s advisable to stay indoors or limit outdoor activities. You can check local air quality reports for guidance.
- Indoor Pollutants: Ensure good ventilation in your home. Avoid using products that release fumes, such as certain cleaning agents or paints. Consider using natural or fragrance-free products.
- Occupational Hazards:
- If your job exposes you to dust, chemicals, or other respiratory irritants, it’s essential to take precautions. This might include wearing protective masks or ensuring proper ventilation in the workspace.
-
Household Irritants:
- Pet Dander: If you have pets, regular grooming and cleaning can reduce dander. Consider using air purifiers to reduce allergens.
- Mold and Mildew: These can be particularly harmful. Ensure that your living spaces are well-ventilated and dry. Use dehumidifiers in damp areas and fix any leaks promptly.
-
Wood Smoke and Open Fires:
- While they might be cozy, wood-burning stoves, fireplaces, and open fires can release particles that can irritate the lungs. If you must be around them, ensure the area is well-ventilated.
-
Vehicle Emissions:
- If you live near a busy road or highway, keep windows closed during peak traffic times. When in a car, use the recirculate air option to reduce exposure to exhaust.
-
Protective Measures:
- Consider wearing a mask, especially on days with high pollution or when exposed to potential irritants.
- Invest in high-quality air purifiers for your home, especially for the bedroom, to ensure you’re breathing the cleanest air possible while sleeping.
8. Mental Health:
Living with CF can be emotionally challenging due to the daily care regimen, frequent hospitalizations, and the potential impact on life expectancy. Addressing mental health is paramount for enhancing quality of life.
-
Emotional Challenges:
- Anxiety and Depression: Studies have shown that individuals with CF are at a higher risk of anxiety and depression. Recognizing the symptoms early and seeking treatment is crucial.
- Social Isolation: Due to the risk of cross-infections, individuals with CF might often feel isolated, especially from others with the same condition.
- Body Image Concerns: Issues like low weight, scarring from surgeries, or the use of medical devices can affect self-esteem.
-
Counseling and Therapy:
- Individual Therapy: Regular sessions with a psychologist or counselor can provide coping strategies and emotional support.
- Cognitive Behavioral Therapy (CBT): This evidence-based approach can help individuals change negative thought patterns and behaviors.
- Family Therapy: CF affects the entire family. Therapy can address family dynamics, improve communication, and offer coping strategies.
-
Support Groups:
- CF-specific Groups: Connecting with others who understand the unique challenges of CF can be therapeutic. However, due to cross-infection risks, online platforms might be more suitable.
- General Chronic Illness Groups: These can offer broader perspectives and coping techniques from individuals with various conditions.
-
Mindfulness and Relaxation Techniques:
- Meditation: Regular meditation can reduce stress, improve focus, and promote a positive outlook.
- Deep Breathing Exercises: Apart from physical benefits, they can also help in relaxation and stress reduction.
- Progressive Muscle Relaxation: This technique involves tensing and then relaxing different muscle groups, promoting physical and mental relaxation.
-
Medication:
- Some individuals with CF might benefit from antidepressants or anti-anxiety medications. It’s essential to discuss potential side effects and interactions with CF medications with a healthcare provider.
-
Staying Connected:
- Social Activities: Engaging in hobbies and activities can offer distraction and boost mood.
- Maintaining Relationships: Keeping close ties with friends and family can provide essential emotional support.
- Educational Resources:
- Workshops: Some organizations offer workshops on mental health topics tailored for CF patients.
- Books and Online Resources: There are many resources specifically addressing the emotional challenges of living with CF.
9. Travel Considerations for Individuals with Cystic Fibrosis:
Traveling can be an enriching experience, but for those with CF, it requires additional planning and precautions to ensure safety and health maintenance.
-
Medication and Equipment:
- Packing Essentials: Always pack more medication than you think you’ll need, ideally twice the amount for the trip’s duration. This accounts for potential delays or lost medications.
- Storage: Some medications might need refrigeration. Consider travel-friendly coolers or check with your accommodation in advance about refrigerator access.
- Equipment: If you use devices like nebulizers or airway clearance devices, ensure they’re travel-friendly and have the necessary power adapters for your destination.
-
Air Travel:
- Cabin Air: The dry air in airplane cabins can thicken mucus. Stay hydrated and consider doing airway clearance before and after the flight.
- Security Checks: Inform security about your medications and devices. A doctor’s letter detailing your medical condition and the necessity of your medications/equipment can be helpful.
- Oxygen Needs: If you require supplemental oxygen, check with the airline well in advance about their policies.
-
Destination Research:
- Healthcare Facilities: Know the locations of the nearest hospitals or clinics at your destination that can cater to CF needs.
- Climate: Different climates can affect CF symptoms. Humid climates might make breathing more difficult, while cold air might be irritating to the lungs.
-
Accommodation:
- Cleanliness: Ensure your accommodation is clean to minimize infection risks. Consider packing disinfectant wipes to clean surfaces.
- Facilities: Check if your accommodation has facilities like a microwave (for sterilizing equipment) or a refrigerator.
-
Avoiding Infections:
- Water Safety: In some destinations, tap water might not be safe to drink. Use bottled water for drinking and for rinsing any equipment.
- Crowds: Crowded places can increase the risk of catching infections. Consider wearing a mask or avoiding peak times.
-
Travel Insurance:
- Coverage: Ensure your travel insurance covers pre-existing conditions and any potential CF-related complications.
- Emergency Evacuation: Consider policies that include emergency evacuation in case of severe health issues.
-
Dietary Needs:
- Food Safety: Be cautious about where and what you eat. Avoid street food or uncooked foods in areas where food safety might be a concern.
- Enzymes: If you take enzymes with your meals, remember to adjust the timing based on the time zone changes.
-
Activity and Rest:
- Pacing: While it’s tempting to see and do everything, remember to pace yourself. Schedule rest periods and continue with your regular treatments.
- Physical Activities: If you’re planning physical activities, ensure they’re within your capability and adjust your treatments if necessary.
10. Stay Informed:
Staying updated with the latest information, research, and advancements in CF care is crucial for patients and their caregivers. Here’s why and how:
-
Understanding the Disease:
- The more you know about CF, the better equipped you are to manage it. This includes understanding the genetics, how it affects the body, and potential complications.
-
Latest Treatment Options:
- Medical research is ongoing, and new treatments or modifications to existing treatments are continually being developed. Being informed means you can discuss these options with your healthcare provider.
-
Clinical Trials:
- Many CF patients opt to participate in clinical trials for new treatments. Staying informed helps you learn about these opportunities, the potential risks, and benefits.
-
Technological Advancements:
- From wearable devices that monitor lung function to apps that help track medication schedules, technology plays a significant role in modern CF care.
-
Dietary and Nutritional Updates:
- As research progresses, there may be new recommendations or findings about the role of diet and nutrition in CF management.
-
Connecting with the CF Community:
- Engaging with local or online CF communities can be a source of support and information. Sharing experiences and tips can be invaluable.
-
Attending Workshops and Conferences:
- Many organizations hold workshops, webinars, and conferences about CF. These events often feature experts in the field and provide a platform for learning and discussion.
-
Subscribing to Newsletters and Journals:
- Many CF foundations and research institutions release regular publications. These can be a reliable source of the latest research and news.
-
Advocacy and Policy Changes:
- Being informed about policy changes can impact access to care, insurance coverage, and more. Advocacy can also play a role in shaping these policies.
-
Mental and Emotional Well-being:
- New research and insights into the psychological impact of living with CF can offer strategies for coping and improving mental health.
11. Plan for the Future:
-
Reproductive Health and Family Planning:
- Fertility Considerations: Men with CF are often infertile due to absent or blocked vas deferens, while women may have reduced fertility. It’s essential to discuss these issues with a fertility specialist to understand options and potential treatments.
- Pregnancy: Women with CF can have successful pregnancies, but they may be at a higher risk for complications. Pre-conception counseling with a CF specialist and an obstetrician experienced in high-risk pregnancies is crucial.
-
Financial Planning:
- Insurance: Ensure you have comprehensive health insurance that covers CF treatments, medications, and hospitalizations. Explore supplemental insurance options that might cover out-of-pocket expenses.
- Special Needs Trusts: These are designed for individuals with chronic illnesses or disabilities. They allow assets to be held in trust, which can be used for the beneficiary’s benefit without affecting eligibility for certain government benefits.
- Retirement Planning: Given the advancements in CF care and increasing life expectancy, planning for retirement is essential. Consider starting early with savings and investments.
-
Advanced Healthcare Directives:
- Living Will: This document specifies what medical actions should be taken if someone is no longer able to make decisions due to illness or incapacity.
- Medical Power of Attorney: Appoint a trusted individual to make medical decisions on your behalf if you’re unable to do so.
- Organ Donation: Some individuals with CF consider registering as organ donors, especially for organs not affected by CF.
-
Career and Education:
- Workplace Accommodations: Understand your rights under laws like the Americans with Disabilities Act, which may provide certain accommodations in the workplace.
- Educational Support: For younger individuals, ensure that schools provide necessary accommodations, such as allowing for frequent breaks or having a place to store and take medications.
-
End-of-Life Planning:
- Funeral Arrangements: While it’s a difficult topic, some individuals find peace in pre-planning funeral arrangements or discussing their wishes with loved ones.
- Legacy Projects: Some people with CF choose to undertake projects or create memories that serve as a legacy, such as writing a memoir, creating art, or recording messages for loved ones.
12. Stay Positive:
A positive mindset can significantly impact one’s overall well-being, especially when managing a lifelong condition like CF. Here’s why it’s essential and how to cultivate it:
-
The Power of Positivity:
- Physical Health Benefits: A positive outlook can boost the immune system, reduce stress hormones, lower blood pressure, and improve cardiovascular health.
- Mental Health Benefits: Positivity is linked to reduced symptoms of depression, lower levels of distress, better psychological well-being, and improved coping skills.
-
Strategies to Foster Positivity:
- Gratitude Journaling: Regularly jotting down things you’re grateful for can shift focus from challenges to blessings. Even small moments of joy can make a difference.
- Limit Negative Inputs: Be mindful of the content you consume, whether it’s news, social media, or entertainment. Surround yourself with uplifting and positive content.
- Mindfulness and Meditation: These practices can help anchor you to the present moment, reduce anxiety, and cultivate a peaceful mind.
- Positive Affirmations: Repeating positive statements can rewire the brain to believe and act upon them. Phrases like “I am resilient” or “I can handle this” can be powerful.
- Seek Inspiration: Read stories or watch documentaries about individuals who have overcome challenges. Their journeys can offer motivation and perspective.
- Engage in Activities You Love: Whether it’s a hobby, sport, or simply spending time in nature, doing things you enjoy can elevate your mood and provide a break from daily stresses.
- Connect with Supportive Communities: Whether it’s a CF support group, a hobby club, or a spiritual community, being around supportive individuals can provide encouragement and understanding.
- Seek Professional Help: Therapists or counselors can offer strategies to manage negative thoughts and feelings. They provide a safe space to express and process emotions.
-
Challenges are Part of Growth:
- Recognize that challenges, setbacks, and difficult days are a part of life. They don’t define you but offer opportunities for growth and learning. Embracing this perspective can make challenges feel less daunting.
-
Celebrate Small Wins:
- Every step forward, no matter how small, is progress. Celebrate your achievements, whether it’s a successful therapy session, a day without symptoms, or even just getting out of bed on a tough day.
-
Final Thoughts
Living with Cystic Fibrosis (CF) is undeniably challenging, but with the advancements in medical research and the growing understanding of the disease, there’s more hope now than ever before. It’s essential for individuals with CF and their families to remember that they are not alone on this journey. Numerous support groups, dedicated healthcare professionals, and fellow CF warriors are out there, offering a helping hand and a listening ear.
Staying informed, proactive, and positive can make a significant difference in managing the disease. While CF does impose certain limitations, it doesn’t define who you are. With determination, resilience, and the right care, individuals with CF can lead meaningful, fulfilling lives, achieving their dreams and inspiring others along the way.
Remember, every challenge presents an opportunity for growth. Embrace the journey, celebrate the small victories, and always hold onto hope.
-
Sources
- Cystic Fibrosis Canada. (n.d.). Living with Cystic Fibrosis. Retrieved November 1, 2023, from https://www.cysticfibrosis.ca/about-cf/living-with-cystic-fibrosis
- National Heart, Lung, and Blood Institute. (n.d.). Living With Cystic Fibrosis. Retrieved November 1, 2023, from https://www.nhlbi.nih.gov/health/cystic-fibrosis/living-with
- Cystic Fibrosis Trust. (n.d.). Life with Cystic Fibrosis. Retrieved November 1, 2023, from https://www.cysticfibrosis.org.uk/life-with-cystic-fibrosis
- American Association for Respiratory Care. (n.d.). Canadian CF Study Results. Retrieved November 1, 2023, from https://www.aarc.org/canadian-cf-study-results/